I have had the luxury of working at my facility for nearly 22 years. I started out as a Care Assistant, and held that title until I graduated with my BSN. I know people who don’t work in healthcare prior or during nursing school. I feel they are disadvantaged. It was in my position at the “bottom” so to speak, that helped me see the things I did and did not want to model. I had nurses who would tell me “I changed that kid’s diaper. It is laying in the crib. Since that is your job, I left it for you to weigh.” Wow, talk about being told your place, I thought we were a team here? On the flip side, I had nurses who would walk out of their way to have me help them hold for an IV. They did this just so they could talk me through pointers that were valuable teaching points. I learned pretty soon, that I wanted to be the second nurse…and I didn’t like to be micro-managed. I would not do that to others. I believe strongly that you can tell by actions those who were and were not CA’s prior to their nursing career.
Someday we will find the answers...maybe
Hi, my name is Joleene and I am not a perfect nurse. (Hi Joleene!) I have made errors in my career. Big errors, small errors, errors I didn’t even know about until someone else told me much later. My big error was a result of multiple fails that fell through a few departments. I missed my opportunity though; I failed and end result was my fault. My patient ended up being safe, but the processes that led to this error were not. I was unfortunate to have a leader that was more interested in the failure than the events that led to the failure. She told me that she was too angry to talk to me, so I would have to deal with someone else.
So one weekday afternoon I sobbed my way into the Chief Nursing Officer’s office and told her my story as I shook. I was relieved when her response was “What do you think is ONE thing we could change about this system to prevent this from happening again?” I remember telling her, “Well…I actually have thought about several things. I can’t get this out of my head.” As I spoke, she took notes, and would comment on feasibility. She ended by telling me “Thank you for not being afraid to admit your error and to help us learn from it”. A weight was lifted. Over the next six months or so, most of my suggestions were put into place. I feel a bittersweet pride about that. I personally experienced a tale of two leaders in that one experience. One was seeing the world via a concrete lens and the other through a complex adaptive system view. There is no doubt that I am/plan on being the second leader. If one falls, we all fall. The best way to prevent that is to find what tripped us up.
We, as an industry, must work towards minimizing interruptions. We also need to show that we are aware the role staffing and triaging our tasks play in our job to help prevent errors. As I watched the section on “Just Culture” I was moved, especially by Annie’s Story (2014) Transparency, Compassion, and Truth in Medical Errors: Leilani Schweitzer (2013). Those stories were me. I was the nurse who had made an error, and I was a part of the journey to make it right. Mandatory reporting is a tool to help make it right if used in the right context, or rather, depending on how it is marketed. We need to stress to staff that we are learning from our mistakes, and we need to know what to change. People feel more open to share when they know we are trying to listen. If we just say we need to report any and all events that occur, people feel vulnerable. I have had nurses tell me that their manager would discipline them when they put in incident reports. They decided just not to tell anyone. Wow! That is a bigger problem. We can’t know what it is that we don’t know, so we are shooting ourselves in the foot if we take that route. I was also surprised that the state of Kansas does not report adverse events. The failure to do this results in lack of transparency to the Kansas healthcare consumer — not to mention that it is hindering our ability to move towards a more complex adaptive system. Come on Kansas, get your head in the game! (To be fair, those last words were uttered by me during this week’s loss to OU…my husband’s team).
So one weekday afternoon I sobbed my way into the Chief Nursing Officer’s office and told her my story as I shook. I was relieved when her response was “What do you think is ONE thing we could change about this system to prevent this from happening again?” I remember telling her, “Well…I actually have thought about several things. I can’t get this out of my head.” As I spoke, she took notes, and would comment on feasibility. She ended by telling me “Thank you for not being afraid to admit your error and to help us learn from it”. A weight was lifted. Over the next six months or so, most of my suggestions were put into place. I feel a bittersweet pride about that. I personally experienced a tale of two leaders in that one experience. One was seeing the world via a concrete lens and the other through a complex adaptive system view. There is no doubt that I am/plan on being the second leader. If one falls, we all fall. The best way to prevent that is to find what tripped us up.
We, as an industry, must work towards minimizing interruptions. We also need to show that we are aware the role staffing and triaging our tasks play in our job to help prevent errors. As I watched the section on “Just Culture” I was moved, especially by Annie’s Story (2014) Transparency, Compassion, and Truth in Medical Errors: Leilani Schweitzer (2013). Those stories were me. I was the nurse who had made an error, and I was a part of the journey to make it right. Mandatory reporting is a tool to help make it right if used in the right context, or rather, depending on how it is marketed. We need to stress to staff that we are learning from our mistakes, and we need to know what to change. People feel more open to share when they know we are trying to listen. If we just say we need to report any and all events that occur, people feel vulnerable. I have had nurses tell me that their manager would discipline them when they put in incident reports. They decided just not to tell anyone. Wow! That is a bigger problem. We can’t know what it is that we don’t know, so we are shooting ourselves in the foot if we take that route. I was also surprised that the state of Kansas does not report adverse events. The failure to do this results in lack of transparency to the Kansas healthcare consumer — not to mention that it is hindering our ability to move towards a more complex adaptive system. Come on Kansas, get your head in the game! (To be fair, those last words were uttered by me during this week’s loss to OU…my husband’s team).
This week, we watched the video from Gawande on healing medicine/healthcare. This video in my opinion is the bridge between the two ideas we focused on this week. It pointed out that in order to have value, we need to see where we can cut some unnecessary things. Gawande (2012) used the example of counting the number of CT that were done and compare them to the number that they found positive. They were giving a lot of unnecessary radiation to people — that can in-turn cause harm. By looking at outcomes, they found what changes they did need, and it turns out it can be as simple as a checklist.
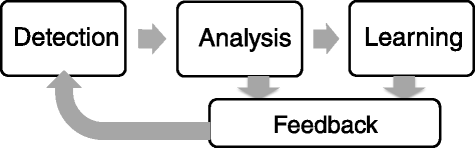
As I watched Ebright’s videos (2010) I became more and more aware that my facility was in fact trending towards a new-age leadership system. We are deep into our Lean journey to identify areas of opportunity, evaluate what makes them opportunities, gather input from all areas to come up with solutions and then put them into action. We don’t stop there though. We re-evaluate, modify, and trial again. Rinse and repeat. We have and will continue to see growth, I have no doubt. I am proud to be a part of leadership here during this time. It is helping to create a mindset of change as good practice. As a leader it helps to know that we are on the right path to the future.